Welcome to Dementia World elderly home services


Dementia affects millions worldwide, gradually robbing individuals of their cognitive abilities and independence. As this condition becomes increasingly prevalent in our aging population, one question persistently emerges: is dementia reversal possible? While traditional medical wisdom has long held that dementia is an irreversible condition, emerging research and clinical observations suggest a more nuanced reality. This article explores the latest scientific findings on potential dementia reversal strategies, from cutting-edge medical interventions to evidence-based lifestyle modifications that may slow or even partially reverse cognitive decline.
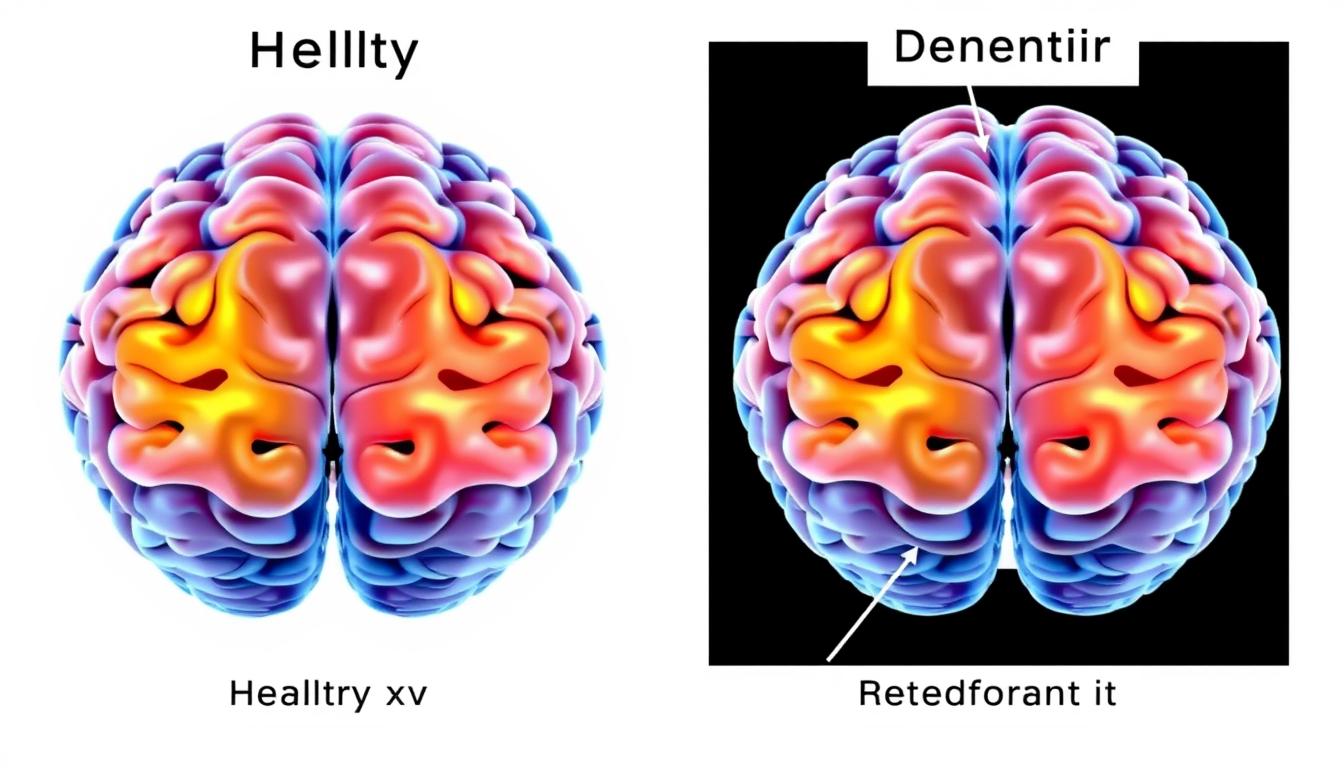
Brain imaging reveals structural differences between healthy brains and those affected by dementia
Dementia is not a single disease but rather an umbrella term describing a collection of symptoms affecting memory, thinking, and social abilities severely enough to interfere with daily functioning. Alzheimer’s disease accounts for 60-80% of cases, while vascular dementia, Lewy body dementia, and frontotemporal dementia represent other common types.
The condition typically progresses through stages, from mild cognitive impairment to severe dementia. Understanding this progression is crucial when discussing potential reversal strategies, as interventions that work at one stage may be ineffective at another.
Important: While true dementia involves progressive neurodegeneration, some conditions can mimic dementia symptoms yet are potentially reversible. These include vitamin deficiencies, medication side effects, thyroid problems, and normal pressure hydrocephalus. Always consult a healthcare provider for proper diagnosis.
Recent scientific advances have challenged the notion that dementia is always irreversible. While complete reversal remains elusive for conditions like Alzheimer’s disease, several promising research directions suggest partial improvement may be possible.

Amyloid plaques are a hallmark of Alzheimer’s disease. Recent clinical trials of medications targeting these plaques have shown mixed results:
These medications represent important advances but come with significant limitations, including potential side effects like brain swelling and microhemorrhages. They also work best in early disease stages and don’t address other dementia types.
Tau protein tangles represent another key pathological feature of Alzheimer’s disease. Several experimental treatments targeting tau are in development:
While still primarily in early clinical trials, these approaches show promise for addressing a crucial aspect of neurodegeneration not targeted by anti-amyloid therapies.
New dementia treatments are constantly being researched. Consider learning about or participating in clinical trials to access cutting-edge treatments.

Non-invasive brain stimulation techniques have emerged as promising approaches for enhancing cognitive function in dementia patients. These methods work by modulating neural activity in specific brain regions.
TMS uses magnetic fields to stimulate nerve cells in targeted brain areas. Multiple studies have investigated its potential for improving cognition in dementia:
While results are promising, effects are often temporary, requiring ongoing treatment sessions to maintain benefits.
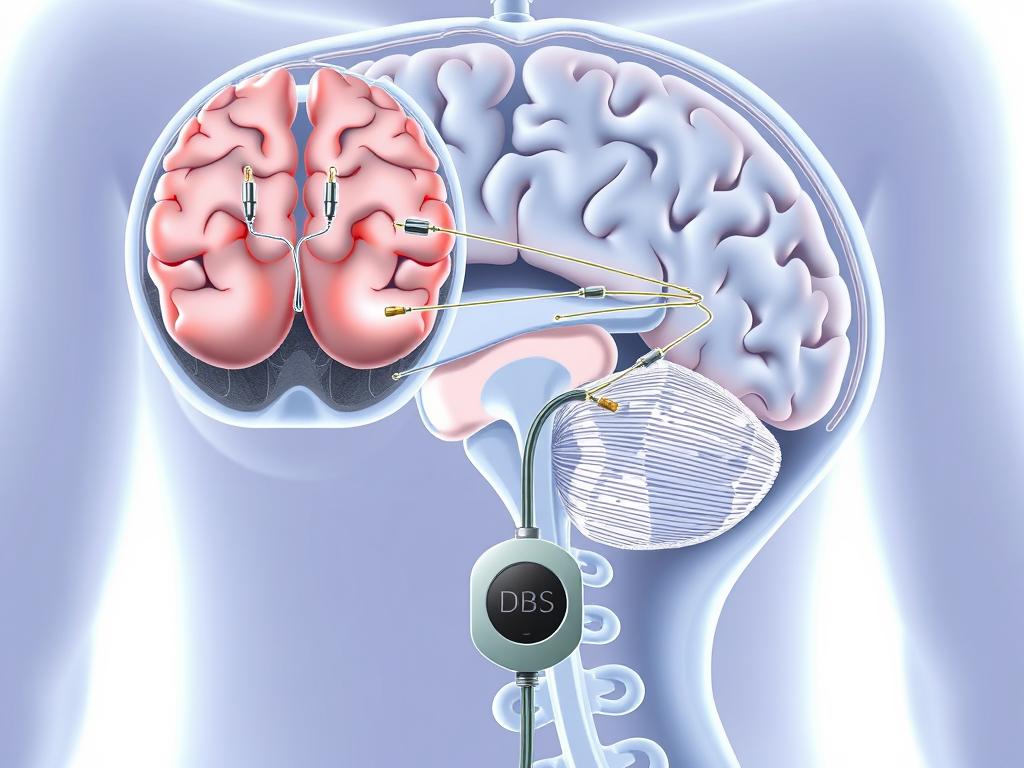
DBS involves surgically implanting electrodes in specific brain regions to deliver electrical stimulation. Originally developed for movement disorders like Parkinson’s disease, DBS is now being investigated for dementia:
DBS represents a more invasive approach with surgical risks but may offer longer-lasting benefits for selected patients.
tDCS applies a low-intensity electrical current to the scalp to modulate brain activity. This relatively simple, portable technology has shown potential for cognitive enhancement:
Important Safety Note: Brain stimulation therapies should only be administered by qualified healthcare professionals. These treatments are still considered experimental for dementia and may not be covered by insurance. Always consult with a neurologist or geriatric specialist before pursuing these options.
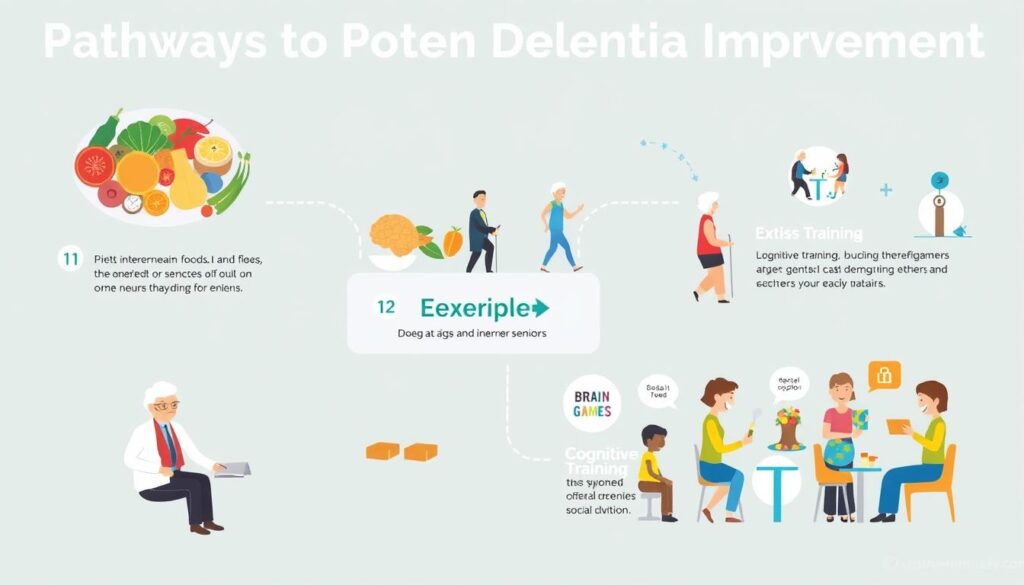
Comprehensive lifestyle interventions target multiple pathways that influence brain health
Some of the most promising evidence for dementia reversal comes from comprehensive lifestyle interventions. These approaches recognize that brain health is influenced by multiple factors and aim to address them simultaneously.
The Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER) represents one of the most rigorous studies of lifestyle intervention for cognitive health. This two-year randomized controlled trial demonstrated that a multi-domain approach could significantly improve or maintain cognitive function in at-risk older adults.
The FINGER protocol includes:
The FINGER study found that participants following this protocol showed a 25-30% improvement in cognitive performance compared to the control group. Similar approaches are now being tested worldwide through the World-Wide FINGERS network.
Developed by neurologist Dr. Dale Bredesen, this personalized approach aims to identify and address multiple factors contributing to cognitive decline. The protocol has generated both interest and controversy in the medical community.
Key components include:
Case studies published by Bredesen and colleagues report cognitive improvement in patients with mild cognitive impairment and early Alzheimer’s disease. However, larger controlled trials are needed to validate these findings.
“The key insight is that dementia is not a single condition with a single cause requiring a single treatment. It’s a complex syndrome requiring a personalized, multi-factorial approach.”
– Dr. Richard Isaacson, Director of the Alzheimer’s Prevention Clinic at Weill Cornell Medicine
Before starting any intensive lifestyle protocol, consult with a healthcare provider specializing in cognitive health to develop a personalized plan.

Diet plays a crucial role in brain health and may influence the progression of dementia. Research increasingly supports specific dietary patterns and nutrients that may help preserve cognitive function.
The MIND diet combines elements of the Mediterranean and DASH (Dietary Approaches to Stop Hypertension) diets, specifically focusing on foods that support brain health.
Research published in Alzheimer’s & Dementia found that strict adherence to the MIND diet was associated with a 53% reduced risk of Alzheimer’s disease, while even moderate adherence reduced risk by 35%.

While a whole-food diet is preferable, certain supplements may help address specific deficiencies or provide therapeutic doses of beneficial compounds:
| Nutrient/Supplement | Potential Benefits | Research Evidence | Considerations |
| Vitamin B12 | Supports myelin formation; reduces homocysteine levels | Deficiency linked to cognitive impairment; supplementation may improve cognition in deficient individuals | Common deficiency in older adults; blood testing recommended |
| Omega-3 Fatty Acids | Anti-inflammatory; supports neuron membrane health | Mixed results in clinical trials; may be most beneficial in early stages | Quality and dosage matter; fish oil supplements should be pharmaceutical grade |
| Vitamin D | Neuroprotective; supports immune function | Low levels associated with increased dementia risk; supplementation benefits unclear | Blood testing recommended; optimal levels may vary by individual |
| Curcumin | Anti-inflammatory; may reduce amyloid and tau accumulation | Promising in animal studies; human trials show mixed results | Poor bioavailability; formulations with enhanced absorption recommended |
| Antioxidants (Vitamins C, E) | Reduce oxidative stress and inflammation | Observational studies suggest benefits; intervention trials less conclusive | Food sources preferable to supplements; high-dose vitamin E controversial |
Supplement Safety Note: Dietary supplements are not regulated as strictly as medications. Always consult with a healthcare provider before starting any supplement regimen, especially if you’re taking other medications. More is not always better, and some supplements can interact with medications or have adverse effects at high doses.

Exercise consistently emerges as one of the most powerful interventions for brain health. Regular physical activity has been shown to:
Research suggests that combining different types of exercise provides the greatest cognitive benefits:
A landmark study published in the Journal of Alzheimer’s Disease found that older adults who engaged in regular aerobic exercise showed increased hippocampal volume (a brain region crucial for memory) and improved memory performance after just six months.
“Exercise is the closest thing we have to a miracle drug for brain health. It’s a powerful intervention that benefits virtually every aspect of brain function.”
– Dr. Wendy Suzuki, Professor of Neural Science and Psychology at New York University
For those new to exercise or returning after a long break, these guidelines can help ensure safety and success:
Many community centers and fitness facilities offer specialized exercise programs for older adults, including those with cognitive concerns.

The concept of “use it or lose it” applies to brain health. Engaging in mentally stimulating activities helps build cognitive reserve—the brain’s resilience to damage—and may enhance neuroplasticity, the brain’s ability to form new connections.
Research has identified several cognitive training methods that show promise for maintaining or improving cognitive function:
Specialized computer programs and apps designed to target specific cognitive domains have shown some benefits:
Low-tech approaches also demonstrate benefits:

Social interaction provides complex cognitive stimulation that cannot be replicated by solo activities. Research consistently shows that social engagement is associated with better cognitive outcomes:
Effective ways to increase social engagement include:
Finding the Right Balance: The most effective cognitive stimulation combines novelty, challenge, and enjoyment. Activities should be difficult enough to require effort but not so challenging that they cause frustration. Variety is important—engaging different cognitive skills through diverse activities provides broader benefits than focusing on a single type of mental exercise.
During deep sleep, the brain’s glymphatic system clears waste proteins, including those linked to dementia
Sleep is far from a passive state for the brain. During sleep, especially deep slow-wave sleep, the brain undergoes crucial maintenance processes that may directly impact dementia risk and progression:
Multiple studies have linked poor sleep quality and sleep disorders with increased dementia risk:
Evidence-based strategies to enhance sleep quality include:
Caution with Sleep Medications: Many sleep medications, particularly benzodiazepines and anticholinergics, may negatively affect cognition and potentially increase dementia risk with long-term use. Non-pharmacological approaches should be tried first, and any medication should be discussed thoroughly with a healthcare provider.

When evaluating claims about dementia reversal, it’s essential to maintain a balanced perspective that acknowledges both promising developments and important limitations.
“We need to be both hopeful and realistic when discussing dementia treatments. While complete reversal of established dementia remains elusive, we now have evidence-based approaches that can slow progression and sometimes improve symptoms, especially when started early. This represents real progress, even as we continue working toward more definitive treatments.”
– Dr. Ronald Petersen, Director of the Mayo Clinic Alzheimer’s Disease Research Center
The field of dementia research faces several ethical challenges:
Future research directions likely to yield important insights include:
While complete reversal of established dementia remains an aspirational goal rather than a current reality, significant progress has been made in understanding how to slow progression and sometimes improve symptoms, especially in early stages. The most promising approaches combine multiple interventions—addressing diet, exercise, sleep, cognitive stimulation, and targeted medical treatments—tailored to individual needs.
For those concerned about cognitive health, the evidence strongly supports being proactive. Early detection of cognitive changes, identification of potentially reversible causes, and implementation of evidence-based lifestyle modifications offer the best opportunity to maintain brain health and function.
As research continues to advance, maintaining a balanced perspective—hopeful but realistic—serves both scientific integrity and the needs of those affected by dementia. The goal is not to create false hope but to empower individuals with accurate information about the most effective strategies currently available while working toward more definitive treatments in the future.
If you’re concerned about cognitive changes in yourself or a loved one, don’t wait to take action. Early assessment and intervention offer the best opportunity for maintaining brain health.
Complete reversal of true dementia, even in early stages, is not currently possible with existing treatments. However, some symptoms may improve with appropriate interventions, and progression can often be slowed. Additionally, some conditions that mimic dementia (such as vitamin B12 deficiency, normal pressure hydrocephalus, or medication side effects) can be reversed with proper treatment. This underscores the importance of comprehensive evaluation by specialists to identify potentially reversible causes of cognitive symptoms.
The Mediterranean and MIND diets have the strongest evidence for supporting brain health. Key foods include leafy greens (like spinach and kale), berries (especially blueberries), fatty fish rich in omega-3s (salmon, mackerel), nuts and seeds, olive oil, and whole grains. These foods provide antioxidants, anti-inflammatory compounds, and nutrients that support neuron health and may help reduce the accumulation of harmful proteins associated with dementia. Equally important is limiting processed foods, added sugars, and excessive alcohol, which may contribute to inflammation and vascular damage.
Some cognitive benefits from lifestyle changes can appear relatively quickly. Aerobic exercise has been shown to improve cognitive processing speed and executive function within 6-12 weeks in some studies. Dietary changes may take longer to show measurable effects, typically 3-6 months. Sleep improvements can enhance memory consolidation almost immediately. However, the most significant benefits come from sustained lifestyle changes over months and years. Consistency is key—sporadic efforts are unlikely to produce meaningful results.
No medications are currently approved specifically for dementia reversal. Existing FDA-approved medications for Alzheimer’s disease (cholinesterase inhibitors like donepezil and memantine) may temporarily improve symptoms or slow progression but do not reverse the underlying disease process. Newer medications like Aducanumab (Aduhelm) and Lecanemab (Leqembi) target amyloid plaques and may slow cognitive decline in early stages, but they do not reverse existing damage. Research continues on more effective treatments, including those targeting tau proteins and neuroinflammation.
Normal aging may include occasional word-finding difficulties, mild forgetfulness (like misplacing items), or taking longer to learn new information. These changes typically don’t interfere significantly with daily functioning. Early dementia signs tend to be more disruptive and may include: forgetting recently learned information, difficulty completing familiar tasks, confusion about time or place, trouble understanding visual images, new problems with words in speaking or writing, misplacing things and inability to retrace steps, decreased judgment, withdrawal from work or social activities, and mood or personality changes. If you’re concerned about cognitive changes, a comprehensive evaluation by a healthcare provider is recommended.