Welcome to Dementia World elderly home services


Have you ever wondered why Alzheimer’s and dementia are often used interchangeably, yet they are not the same? Understanding the distinction between these two conditions is crucial for recognising symptoms and seeking timely help.
Dementia is an umbrella term for a range of conditions affecting the brain, leading to memory loss and cognitive decline. Alzheimer’s, on the other hand, is the most common form of dementia, accounting for 60-80% of cases. While both share similarities, they differ in causes, progression, and treatment options.
This article aims to demystify these terms, explain their key differences, and highlight the importance of early detection. Stay tuned as we explore symptoms, diagnostic insights, and available support resources.
Many people confuse dementia and Alzheimer’s, but they are distinct conditions. While both affect cognitive abilities, they differ in their causes, progression, and treatment. To better understand these conditions, it’s important to define each term clearly.
Dementia is not a single disease but an umbrella term for a group of symptoms affecting memory, thinking, and social abilities. These symptoms interfere with daily life and can have multiple causes. The most common cause of dementia is Alzheimer’s disease, but other conditions like vascular dementia and Lewy body dementia also fall under this category.
Alzheimer’s disease is a specific type of dementia and the most prevalent, accounting for 60-80% of cases. It is a progressive condition characterised by the build-up of amyloid plaques and tau tangles in the brain. These biological changes disrupt communication between brain cells, leading to memory loss and cognitive decline.
While Alzheimer’s is often associated with ageing, it is not a normal part of getting older. The risk increases significantly after the age of 65, though younger-onset cases can occur. Early detection is crucial, as symptoms may appear decades after the initial brain changes.
While Alzheimer’s is a form of dementia, not all dementia is Alzheimer’s. Dementia is an umbrella term for conditions affecting memory, thinking, and social abilities. Alzheimer’s dementia, however, is the most common type, accounting for 60-80% of cases. Understanding these differences is vital for accurate diagnosis and treatment.

Alzheimer’s dementia is characterised by the build-up of amyloid plaques and tau tangles in the brain. These changes disrupt communication between brain cells, leading to memory loss and cognitive decline. Unlike other forms of dementia, Alzheimer’s progresses gradually, with symptoms worsening over time.
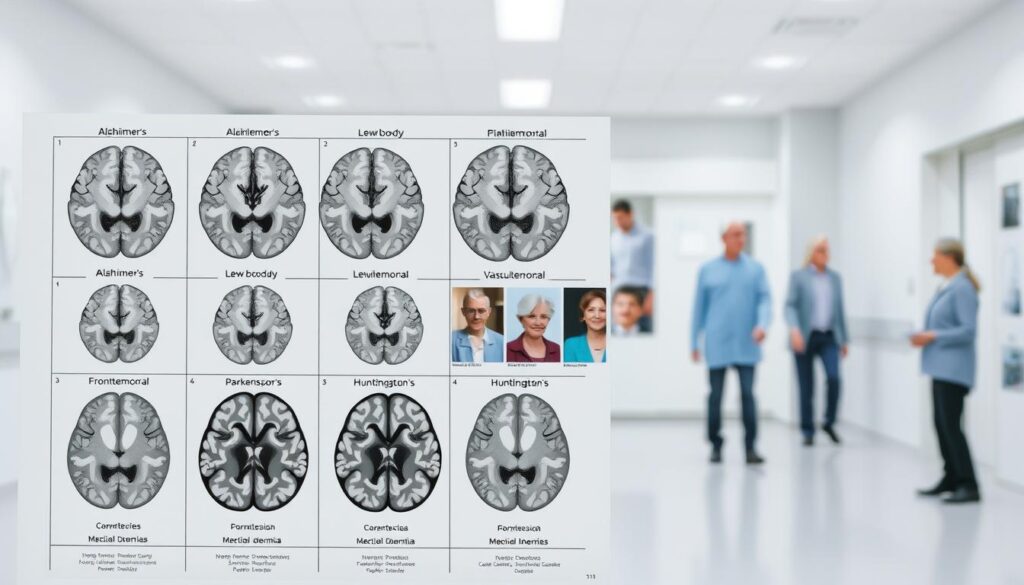
Other types of dementia include vascular dementia, Lewy body dementia, and frontotemporal dementia. Vascular dementia is caused by reduced blood flow to the brain, often following a stroke. Lewy body dementia is marked by visual hallucinations and movement issues. Frontotemporal dementia primarily affects behaviour and language.
Rare forms, such as posterior cortical atrophy, focus on vision and spatial difficulties. Accurate diagnosis is crucial, as each type requires tailored treatment. Recognising the symptoms alzheimer and understanding the cause dementia can help in managing the condition effectively.
Recognising the early signs of Alzheimer’s disease can make a significant difference in managing the condition. The symptoms alzheimer disease often start subtly and worsen over time, affecting memory, thinking, and behaviour. Early detection is crucial for planning care and support.

In the initial stages, individuals may experience mild cognitive impairment (MCI), which can be a precursor to Alzheimer’s. Common signs symptoms alzheimer include difficulty recalling recent events, misplacing items, and asking repetitive questions. Other red flags include forgetting conversations or struggling with familiar tasks like cooking or managing finances.
As the disease progresses, symptoms become more pronounced. Memory loss intensifies, and individuals may struggle with language, reasoning, and problem-solving. Behavioural changes such as agitation, personality shifts, and social withdrawal often emerge. In the late stages, individuals may lose the ability to speak, move, or recognise loved ones.
On average, life expectancy post-diagnosis ranges from 4 to 8 years, though this varies depending on individual health and care. Understanding the decline associated with Alzheimer’s can help families prepare for the challenges ahead.
Dementia manifests in various ways, each type presenting unique challenges. While some symptoms are shared across different forms, others are specific to certain types. Recognising these differences is crucial for accurate diagnosis and tailored care.
Many forms of dementia share similar symptoms, such as memory loss, confusion, and mood swings. These issues often interfere with daily life, making tasks like managing finances or remembering appointments difficult. Additionally, changes in thinking and problem-solving abilities are common across the board.
Each type of dementia has its own distinct features. For example, Lewy body dementia often includes visual hallucinations and sleep disturbances. Frontotemporal dementia primarily affects behaviour and language, leading to impulsivity and language deficits. Vascular dementia, caused by reduced blood flow to the brain, shows a “stepwise” decline after strokes.
| Type of Dementia | Common Symptoms | Unique Symptoms |
|---|---|---|
| Lewy Body Dementia | Memory loss, confusion | Visual hallucinations, sleep disturbances |
| Frontotemporal Dementia | Mood swings, thinking problems | Language deficits, impulsivity |
| Vascular Dementia | Memory loss, confusion | Stepwise decline after strokes |
Understanding these symptoms is vital for effective management. Tailored strategies can help address specific challenges, improving quality of life for those affected. Early recognition and intervention are key to providing the right support.
Accurate diagnosis is the cornerstone of managing cognitive decline effectively. Identifying the specific condition behind memory problems ensures tailored treatment and support. The process often begins with a GP referral to a memory clinic for a comprehensive assessment.

Diagnosing Alzheimer’s involves several steps. First, a detailed medical history is taken to understand the progression of symptoms. Blood tests are conducted to rule out reversible causes, such as vitamin deficiencies or thyroid issues.
Brain imaging, like MRI or CT scans, helps identify structural changes. Neuropsychological exams assess cognitive functions, including memory and problem-solving. Biomarker tests, such as amyloid PET scans and cerebrospinal fluid (CSF) analysis, detect amyloid plaques and tau tangles, key indicators of Alzheimer’s.
Lumbar punctures are sometimes used to analyse CSF for these proteins. Challenges arise in diagnosing atypical variants, which may not present with classic symptoms. Early and precise diagnosis is crucial for effective management.
Diagnosing other forms of dementia follows a similar pathway but focuses on specific markers. For example, vascular dementia is often linked to stroke history, while Lewy body dementia may involve visual hallucinations and sleep disturbances.
Frontotemporal dementia is identified through behavioural and language changes. UK-specific pathways, such as NHS memory services, provide structured support. Ruling out reversible causes remains a priority in all cases.
| Type of Dementia | Diagnostic Methods | Key Indicators |
|---|---|---|
| Alzheimer’s | Amyloid PET scans, CSF analysis | Amyloid plaques, tau tangles |
| Vascular Dementia | Brain imaging, stroke history | Reduced blood flow |
| Lewy Body Dementia | Clinical evaluation, sleep studies | Visual hallucinations |
| Frontotemporal Dementia | Behavioural assessment, language tests | Behavioural changes |
Understanding the diagnostic process helps in managing health effectively. Early intervention can significantly improve quality of life for those affected. Tailored strategies ensure the right support is provided at every stage.
Understanding the risk factors for cognitive decline is essential for prevention and early intervention. While some factors, like age and genetics, cannot be changed, others, such as lifestyle choices, can be managed to reduce the likelihood of developing these conditions.
Age is the strongest non-modifiable risk factor. After 65, the chance of developing cognitive issues doubles every five years. Genetics also play a significant role. For instance, the APOE-e4 gene increases the likelihood of memory-related conditions. In rare cases, familial links can lead to early-onset issues.
Modifiable risk factors include smoking, high blood pressure, and a sedentary lifestyle. Cardiovascular health is closely tied to brain health, as conditions like hypertension can increase the risk. In the UK, factors such as air pollution, poor diet, and social isolation also contribute to cognitive decline.
Proactively managing diabetes and obesity can further reduce risks. Regular exercise, a balanced diet, and mental stimulation are practical steps to support brain health. Addressing these factors early can make a significant difference in long-term outcomes.
The brain undergoes significant changes when affected by cognitive conditions. These alterations disrupt communication between neurons, leading to memory loss and cognitive decline. Understanding these processes is crucial for developing effective treatments.
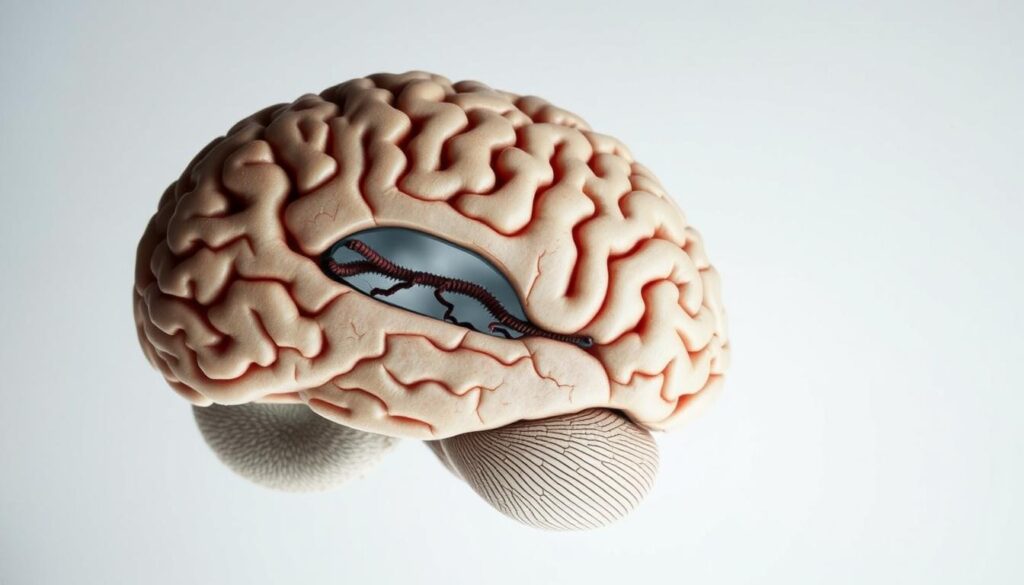
Two key factors in brain deterioration are plaques tangles. Amyloid plaques form in the synaptic spaces between neurons, blocking communication. Tau tangles, on the other hand, destabilise cell structures, leading to neuronal death.
These changes begin in the hippocampus, the brain region responsible for memory. Over time, they spread to the cortex, affecting thinking and behaviour. The severity of symptoms often correlates with the extent of neuronal damage.
As the condition progresses, the brain shrinks, a process known as atrophy. This shrinkage is most noticeable in advanced stages. Neuronal death accelerates, leading to a decline in cognitive functions.
Research into anti-amyloid drugs, such as lecanemab, offers hope. These drugs aim to reduce the build-up of harmful proteins, potentially slowing disease progression. However, more studies are needed to confirm their long-term effectiveness.
| Brain Region | Impact | Stage |
|---|---|---|
| Hippocampus | Memory loss | Early |
| Cortex | Thinking and behaviour changes | Mid to Late |
| Entire Brain | Shrinkage (atrophy) | Advanced |
Understanding how the brain is affected by these conditions is vital. Early intervention and targeted treatments can help manage symptoms and improve quality of life. Continued research is essential for finding effective solutions.
Managing cognitive conditions requires a combination of medical and lifestyle approaches. Effective treatments aim to slow progression, manage symptoms, and improve quality of life. Both pharmacological and non-pharmacological strategies play a vital role in care.
Several medications are available to manage symptoms and slow decline. Cholinesterase inhibitors, such as donepezil, are commonly prescribed to enhance memory and thinking. Disease-modifying drugs like lecanemab and donanemab target amyloid plaques, showing promise in early-stage conditions.
In the UK, access to these therapies often involves clinical trials or NHS-approved pathways. It’s essential to consult healthcare professionals to determine the most suitable option. Regular monitoring ensures the effectiveness of the chosen treatment.
Beyond medications, supportive care is crucial for managing cognitive conditions. Cognitive stimulation therapy and structured routines help maintain mental agility. Non-pharmacological interventions, such as music therapy and reminiscence work, provide emotional and psychological benefits.
Adopting healthy lifestyle changes can also make a significant difference. Regular exercise, a balanced diet, and mental engagement support overall brain health. Carer training and respite care programmes offer essential support for families, ensuring sustainable caregiving.
Combining these approaches creates a holistic care plan, addressing both the physical and emotional needs of individuals. Early intervention and tailored strategies are key to improving outcomes.
Navigating life with cognitive conditions presents unique challenges for both individuals and their families. Adapting to these changes requires practical adjustments and emotional resilience. Understanding the daily life of those affected can help in providing the right support.
For people living with cognitive decline, everyday tasks can become difficult. Simple activities like cooking or managing finances may require assistance. Home safety modifications, such as installing grab bars or removing tripping hazards, can make a significant difference.
Memory aids, like calendars and reminder apps, help maintain independence. Emotional challenges, such as grief and stigma, are also common. Relationships may shift, requiring open communication and patience from family members.
Caregivers play a crucial role in providing support, but they also need care themselves. Burnout is a real risk, so self-care is essential. Resources like the Alzheimer’s Society’s Dementia Support Line and online forums offer valuable guidance.
In the UK, local authority care assessments ensure individuals receive tailored assistance. Programmes like Carer’s Allowance and Admiral Nurses provide financial and emotional support. Age UK also offers practical advice and services.
Advance care planning, including lasting power of attorney, ensures that individuals’ wishes are respected. This proactive approach can ease the burden on families and improve the quality of life for those affected.
| Resource | Purpose |
|---|---|
| Alzheimer’s Society Support Line | Emotional and practical guidance |
| Carer’s Allowance | Financial support for caregivers |
| Admiral Nurses | Specialist dementia care |
| Age UK | Practical advice and services |
Advancements in cognitive health research are paving the way for groundbreaking treatments and early detection methods. Scientists are making significant strides in understanding the underlying causes of memory-related conditions, offering hope for improved outcomes.
Recent breakthroughs include the development of anti-tau antibodies and inflammation-targeting drugs. These innovations aim to address the biological mechanisms behind cognitive decline. The UK Biobank plays a pivotal role in dementia research, providing valuable data for large-scale studies.
Blood tests for early amyloid detection are also in development, offering a non-invasive method for identifying risks. UK-based studies on lifestyle interventions, such as diet and exercise, highlight the importance of holistic approaches to prevention and management.
Gene therapy and precision medicine are emerging as promising future directions. These approaches aim to tailor treatments to individual genetic profiles, enhancing effectiveness. Ethical considerations in clinical trials are also being addressed to ensure participant safety and informed consent.
Artificial intelligence is predicted to revolutionise early diagnosis through speech pattern analysis. This technology could detect subtle changes in language, enabling earlier intervention. Continued progress in these areas holds the potential to transform cognitive health care.
Taking proactive steps can significantly reduce the likelihood of cognitive decline. By focusing on prevention and understanding risk factors, individuals can take control of their brain health. Simple lifestyle changes and early interventions play a crucial role in maintaining cognitive function.
Adopting a healthy lifestyle is one of the most effective strategies for reducing the risk of cognitive decline. The MIND diet, which combines elements of the Mediterranean and DASH diets, has been linked to slower cognitive decline. This diet emphasises leafy greens, berries, nuts, and whole grains.
Other practical steps include:
Managing hearing loss is also important. Studies show that using hearing aids can reduce the risk of cognitive issues by 8%. Regular hearing checks and addressing hypertension are additional measures to protect brain health.
Early detection of cognitive issues can make a significant difference in managing and preventing further decline. Recognising symptoms early allows individuals to access clinical trials and emerging treatments. In the UK, initiatives like Brain Health Check-ups provide structured assessments to identify risks.
For families with a history of cognitive conditions, genetic counselling can offer valuable insights. Understanding genetic risks enables individuals to take personalised prevention measures. Early diagnosis also allows for better planning and support, improving quality of life for both individuals and their families.
By focusing on early detection and adopting proactive strategies, it’s possible to reduce the impact of cognitive decline and maintain brain health for longer.
Understanding the distinction between cognitive conditions is vital for effective management. While Alzheimer’s is a specific cause, dementia represents the broader outcome of cognitive decline. Recognising early symptoms and seeking timely diagnosis can significantly improve quality of life.
If you or a loved one experience memory concerns, consult a healthcare professional promptly. Early intervention allows access to emerging treatments and tailored care plans. Simple lifestyle changes, such as a balanced diet and regular exercise, can also reduce risks.
Hope lies in ongoing research and community support networks. In the UK, resources like the Alzheimer’s Society and NHS provide valuable guidance and assistance. By staying informed and proactive, we can better navigate these challenges together.